In the same section
- Female Fertility Projects
-
Male Fertility Projects
- 1 The role of ion channels in spermatogenesis and the sperm capacitation process.
- 2.Mathematical modelling and experimental study of the sperm capacitation process
- 3.Impact of capacitation failure in human sperm and the identification of capacitation biomarkers in male infertility.
- 4.Pharmacological protection against chemotherapy damage
- Scientific Activities
- Médecine
- Human Reproduction
- EN
- Activities
- Female fertility
- Fundamental Research
- Cryopreservation
cryopreservation
- Ovarian tissue cryopreservation and transplantation
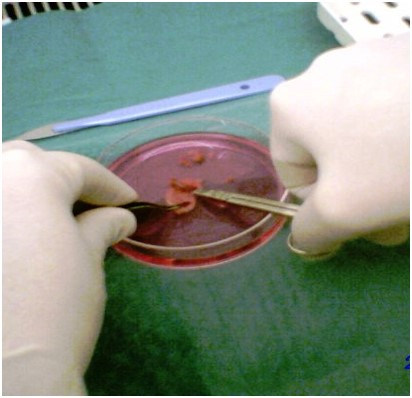
Thanks to recent progress in diagnosis and treatment of cancer, relapse-free survival rate has greatly improved over the last decades. Quality of life of young cancer survivors including access to motherhood, became a major issues. Long-term adverse effects of adjuvant treatments potentially include infertility and premature ovarian failure in around 40% of premenopausal patients. Fertility preservation procedures prior to chemotherapy became the main research axis of our laboratory, including cryopreservation of ovarian tissue and transplantation. The Laboratory first set up a ovarian tissue bank in Erasme Hospital in 1999 and became the reference centers for around 15 oncological units. In 2020, more than 400 patients have benefit from this experimental procedure at Erasme.
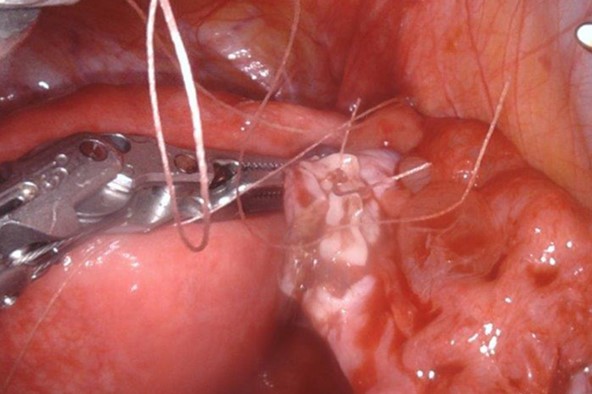
In order to restore ovarian function and fertility, the tissue can be thawed and autotransplanted if premature ovarian failure occurs after treatment. Our laboratory early innovated in this field by obtaining one of the first spontaneous pregnancy and live birth after transplantation of cryopreserved ovarian tissue. However, there are still cases where the transplant remains impossible for the moment. Indeed, in some pathologies with a higher risk of dissemination within organs such as leukemias and non-Hodgkin's lymphomas, the risk of tumor development after grafting remains significant. In other pathologies such as neuro- and medulloblastomas, this risk is not well known. The transplantation of cryopreserved ovarian tissue is not indicated in these cases but unfortunately no alternative is currently available to use this ovarian tissue in order to restore fertility. The laboratory has developed, in collaboration with the Department of Genetics (CUB-Erasme), highly sensitive techniques to allow the detection of these residual cells in the ovarian tissue before transplantation and to ensure its safety.
